Guide By – Los Angeles Nursing Home Infections Attorney
 Proper care and infection prevention practices can prevent infections at long-term care facilities, such as nursing homes and assisted living facilities. Unfortunately, annually, hundreds of thousands of patients die from infections. When an infection occurs, this is frequently a sign of elder abuse & neglect. Understaffing is also a major contributor to facility-acquired infections. A Los Angeles nursing home infections attorney and assisted living infection lawyer, Cherepinskiy Law Firm, will tirelessly advocate for the rights of the infection victims or their families.
Proper care and infection prevention practices can prevent infections at long-term care facilities, such as nursing homes and assisted living facilities. Unfortunately, annually, hundreds of thousands of patients die from infections. When an infection occurs, this is frequently a sign of elder abuse & neglect. Understaffing is also a major contributor to facility-acquired infections. A Los Angeles nursing home infections attorney and assisted living infection lawyer, Cherepinskiy Law Firm, will tirelessly advocate for the rights of the infection victims or their families.
Skilled nursing facilities and assisted living facilities provide services to millions of Americans. Based on the statistical data from the United States Centers for Disease Control and Prevention (“CDC”), the number of nursing home patients exceeds 4 million per year. The number of individuals residing at assisted living facilities is close to 1 million.
Statistics Regarding Infections in the Elderly in Long-Term Care Settings
The CDC’s analysis of the medical literature shows the following statistical data regarding infections in long-term care settings:
- Every year, the residents of long-term care facilities, including nursing homes and assisted living facilities, suffer 1 to 3 million serious infections; and
- Infections play a significant role in patient hospitalizations, extended hospital stays, high morbidity rates and fatal outcomes. In fact, the CDC estimates that, each year, infections cause deaths of approximately 380,000 – over one third of a million – people.
Common Infections in Nursing Homes
 Nursing home patients and residents of assisted living facilities are at a higher risk of infection because of the following factors: the age itself and the resulting weakened immune system, prolonged and frequent hospitalizations, malnutrition, frequent use of antibiotics, impaired mobility and incontinence, as well as impaired cognitive function that leads to poor hygiene.
Nursing home patients and residents of assisted living facilities are at a higher risk of infection because of the following factors: the age itself and the resulting weakened immune system, prolonged and frequent hospitalizations, malnutrition, frequent use of antibiotics, impaired mobility and incontinence, as well as impaired cognitive function that leads to poor hygiene.
Below are some of the most common infections that affect elderly individuals in the long-term care setting.
Clostridium Difficile
Clostridium difficile (often referred to as “C. difficile” or “C. diff”) – is a type of dangerous bacteria, which can cause a variety of serious symptoms ranging from diarrhea to life-threatening colon inflammation. Typically, this bacterial infection occurs among those patients who take antibiotics. Most frequently, illnesses related to C. difficile affect elderly patients in long-term care facilities such as nursing homes and assisted living facilities. Once a patient is infected, if a nursing home or an assisted living facility does not follow proper sanitary protocols, Clostridium difficile can easily spread through the entire facility through contaminated hands, utensils, food surfaces, and medical equipment.
C. diff is associated with an increased morbidity in long-term care facilities. At the turn of the 21st century, the rate of infections almost doubled – from almost 150,000 cases in 2001, to over 300,000 cases in 2005. Elderly patients are the most vulnerable segment of population in terms of the Clostridium difficile, and elders are the most likely to suffer life-threatening consequences of this infection. Some nursing home patients can be “carriers” of the C. diff infection without becoming sick or having any symptoms at all. This means that infected patients can spread the disease to others without any visible physical warning signs. Statistically, out of every 100 nursing home patients, 10 to 20 individuals will become infected with Clostridium difficile.
A C. difficile infection can have dire consequences. In addition to the potential for a serious inflammation of the colon, diarrhea and poor appetite lead to dehydration and malnutrition. The weakening of the immune system results in patients’ susceptibility to subsequent infections. Overall, this infection makes elderly patients weak and frail. During a year following a C. diff infection, patients suffer an increased mortality rate.
Despite the rise in the incidence of the C. diff infections, this is a highly preventable infectious disease. The use of antibiotics must be limited to only those cases where such medications are absolutely necessary, and the administration of antibiotics should be properly supervised and monitored. Similarly, in order to reduce the potential for exposure to other patients, if possible, patients infected with Clostridium difficile should be provided with a private room or, at least, a private bathroom / restroom. In order to prevent the spread of the infection, potential outbreaks, and even fatalities, nursing homes and assisted living facilities must implement appropriate sanitation protocols – the staff has to routinely wash their hands, and all medical equipment and utensils must be cleaned on a regular basis. Disinfecting chemical agents (such as sodium hypochlorite) must also be used to clean potentially contaminated surface areas.
Gastroenteritis
Bacterial and viral gastroenteritis (commonly known as a “stomach flu”) account for the vast majority of outbreaks of diarrhea in nursing homes. The most common gastroenteritis-inducing virus is called “norovirus”, and it causes more than half of all outbreaks of gastroenteritis in the World. This virus is extremely contagious, and it easily spreads through personal contact, as well as through water, food, and other contaminated objects. Due to their decreased ability to produce gastric acid, elderly patients are more susceptible to the development of infectious gastroenteritis. While gastroenteritis is typically not life-threatening, in the older nursing home population, it is associated with a higher rate of morbidity and mortality caused by dehydration.
In the long-term care setting, gastroenteritis outbreaks can last a long time and can affect multiple patients. In order to prevent outbreaks and avoid potential fatalities, nursing homes and assisted living facilities have to implement appropriate sanitation protocols. The staff must utilize proper hand hygiene and, if a staff member gets infected with gastroenteritis, he or she must be prevented from attending to patients. Affected patients have to be isolated from other patients in a private room or, at least, must be provided with a private bathroom / restroom. Chemical disinfecting agents should also be used on a regular basis.
Urinary Tract Infections (UTIs)
A urinary tract infection (UTI) is an infection that is, most commonly, caused by bacteria. In some rare cases, a UTI can be caused by fungi or a virus. UTIs may involve any organ within the urinary tract, including urethra, bladder, ureters, and kidneys.
A urinary tract infection can have multiple symptoms. The most common symptoms include, but are not limited to, the following:
- the feeling of burning during urination
- increased urgency and frequency of urination
- cloudy and discolored urine
- blood in urine
- the presence of a strong odor in urine
- fever and chills
- nausea and vomiting
- upper back pain
In elderly patients, UTIs can lead to the sudden mental state changes, including confusion, agitation, and aggravation of dementia.
In the long-term care setting, particularly in nursing homes, UTI is the most common infection. When patients have an indwelling urinary catheter (a flexible plastic tube that is used to drain urine from the bladder when a patient cannot urinate), the risk of acquiring UTIs and bacteria in the urine increases. In fact, if a urinary catheter is inserted for a month, bacteriuria (the presence of bacteria in the urine) is essentially guaranteed. The increased rate of urinary catheter use, coupled with dehydration, leads to the high incidence of UTIs among elderly patients. Bacterial UTIs have to be treated with a course of antibiotics.
In order to minimize the risk of UTIs related to indwelling urinary catheters, the staff at long-term care facilities must make sure that catheters are used only when they are absolutely necessary. When an assessment shows that the catheter is no longer required, it must be promptly removed. Finally, and most importantly, every time a catheter is inserted or manipulated in any way, the staff must follow proper sanitation procedures, including appropriate hand hygiene and the use of personal protective equipment that includes gloves, masks, and gowns.
Scabies
Besides pressure sores, the one of the most dangerous skin conditions encountered in the nursing home and assisted living setting is a scabies. This skin condition is caused by a parasitic mite which is also commonly referred to as “Sarcoptes scabiei” or “the human itch mite.” Another species of mites called “Scabies crustosa” or “Scabies norvegica” caused a condition entitled “crusted scabies”. Based on the data from the Centers for Diseases Control and Prevention (“CDC”), scabies is an extremely contagious condition where the human itch mite spreads by direct contact with the skin of a person with scabies, as well as by contact with clothing, towels, or bed sheets of an affected person. In order to lay eggs, the mites create tunnels by burrowing into the skin. This causes severe itching, pain, rash, blisters, and under-skin bumps. If this condition is not treated, in some cases, especially in the elderly population, scabies can cause death.
In order to prevent wide-spread epidemics, nursing homes and assisted living facilities must implement appropriate sanitation and infection control protocols as well as the policies and procedure aimed at prompt recognition and rapid treatment of scabies.
Methicillin-Resistant Staphylococcus aureus (MRSA)
Methicillin-resistant Staphylococcus aureus (MRSA) is a type of bacteria that causes a serious infection when it enters a human body through any source, including wounds and cuts, as well as medical devices such as catheters, breathing tubes, and syringes.
Antibiotics can be a powerful medication against bacteria but they cannot treat viruses. Unfortunately, for many years, patients have been prescribed antibiotics even when they were not necessary – i.e. for flu, colds, and other viral infections. Also, since antibiotics are not capable of destroying every single bacteria, those types of bacteria that survived a course of antibiotics become the so-called “drug-resistant bacteria”. MRSA is one of those kinds of drug-resistant bacteria, which is reflected in its name – Methicillin-resistant Staphylococcus aureus. Therefore, MRSA resists the majority of common antibiotics, and this infection has become very difficult and challenging to treat, especially among the elderly. As a result, in the setting of nursing homes and assisted living facilities, MRSA infections can easily lead to epidemics with potentially deadly consequences.
MRSA infections may involve the skin, surgical wounds, bones, joints, lungs and, in the most serious and life-threatening cases – heart valves and the bloodstream. The symptoms of MRSA infections include, but are not limited to, the following:
- fever
- chills
- skin abnormalities such as rash and abscesses
- headaches
- fatigue
- pain in the chest
The treatment of MRSA infections requires very strong IV medications. In the setting of nursing homes and assisted living facilities, where elderly residents have a weak immune system, the infected person may need to be isolated in order to prevent the spread of the infection and the facility-wide epidemic.
Proper hygiene and sanitation protocols, as well as appropriate staff training – are essential in ensuring that facility-acquired MRSA infections are prevented and controlled.
Sepsis
Sepsis is a life-threatening condition, which is caused by a human body’s response to an infection. Sepsis develops when, instead of fighting an infection, the chemicals released by the immune system into a person’s bloodstream – cause an inflammation in the entire body. Based on the data from the Centers for Disease Control and Prevention (“CDC”), every year, over 1.5 million patients get sick with sepsis. In the United States, each year, sepsis causes over 250,000 patient deaths. Due to their weakened immune system, seniors comprise the vast majority of sepsis cases.
Although sepsis can be caused by any infection, the following infections are associated with a higher risk of causing sepsis: infected pressure sores, infections in the bloodstream, abdominal and kidney infections, and pneumonia.
Sepsis is associated with three levels of severity or stages: (1) sepsis, (2) severe sepsis, and (3) septic shock. With sepsis, the infection rapidly spreads through the human body. Severe sepsis can lead to organ failure, blood clots and gangrene. In the worst cases, a patient may suffer a septic shock – a medical emergency, where the patient develops an extremely low blood pressure that can potentially cause the following: stroke; organ failure, including respiratory and heart failure; and even death. In fact, septic shock has a very high mortality rate, and every minute counts when attempts are made to save the patient’s life.
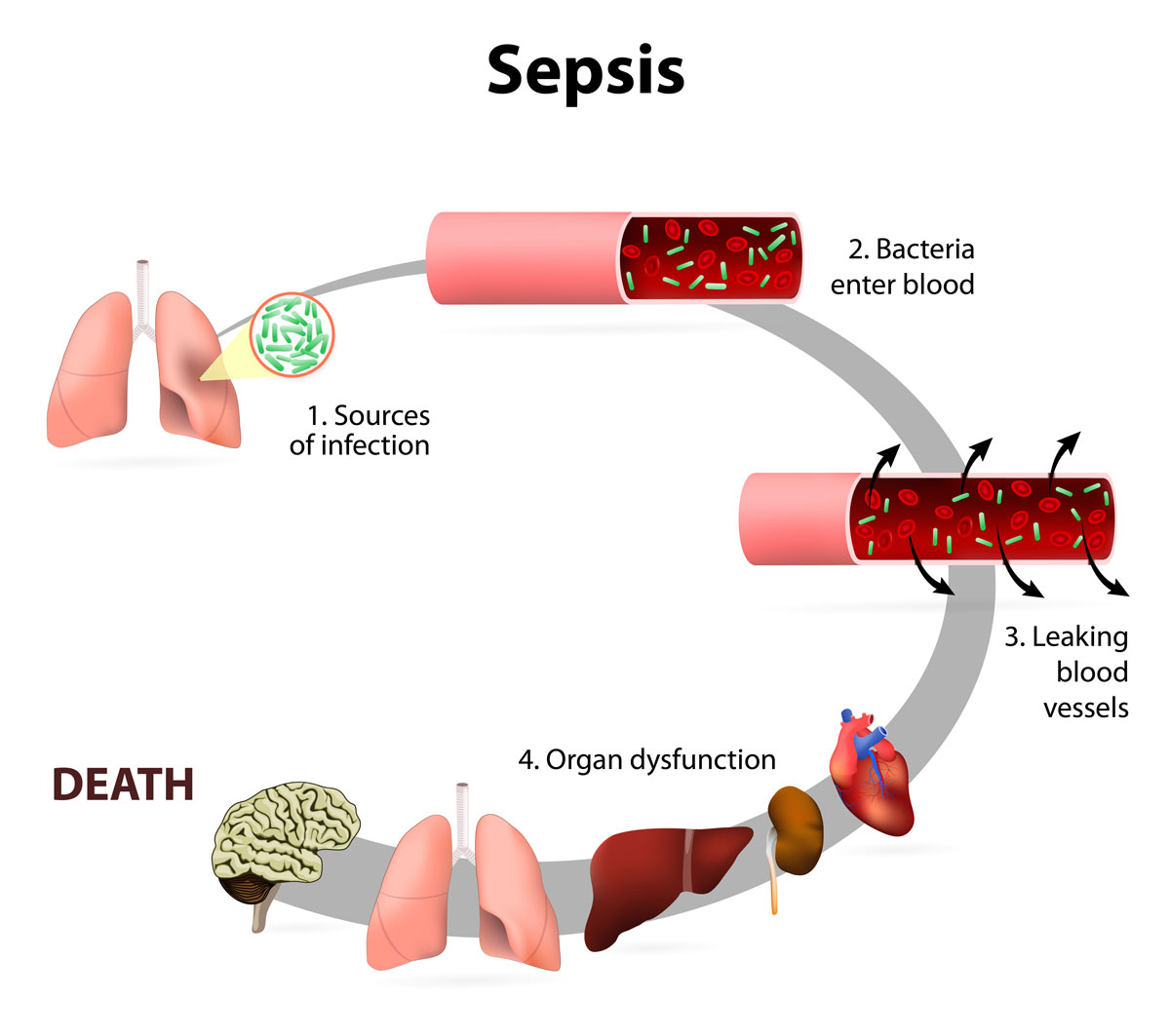
Sepsis is diagnosed when a patient experiences at least two of these symptoms:
- a high fever or a hypothermia (an abnormally low body temperature);
- an abnormally high heart rate (above 90 beats per minute);
- hyperventilation (breathing faster than 20 breaths per minute); and
- an infection.
With severe sepsis, patients exhibit one or more of these symptoms: an altered mental state, decreased urinary output, skin discoloration, respiratory difficulties, cardiac abnormalities, severe weakness, and loss of consciousness.
At long-term care facilities, proper hygiene protocols are essential to reduce the risk of sepsis. Patients must be bathed on a regular basis, encouraged to wash hands and, most importantly, appropriate wound care must be provided whenever an elderly patient has any pressure sores. If a patient is suspected to have developed sepsis, treatment must start immediately – every wasted minute brings a sepsis-affected elderly patient closer to death.
Pneumonia and Influenza
 Pneumonia is an infection, which causes an inflammation in a lung or both lungs. The air sacs in the lung(s) may become inflamed and filled with pus, which then causes difficulty breathing, chills, fever and, most significantly, cough with phlegm or pus.
Pneumonia is an infection, which causes an inflammation in a lung or both lungs. The air sacs in the lung(s) may become inflamed and filled with pus, which then causes difficulty breathing, chills, fever and, most significantly, cough with phlegm or pus.
When an elderly person gets sick with pneumonia, it is very serious matter. Lower respiratory tract infections and pneumonia are the leading cause of death and the main reason for hospitalizations among nursing home residents. In fact, pneumonia is considered to be the fifth leading cause of death in elderly people. In the United States, nursing home patients comprise approximately ten to eighteen percent of all patients hospitalized with pneumonia. Frequently, early signs and symptoms of pneumonia are not timely recognized. If an elderly person’s bacterial pneumonia is left untreated, it can lead to a blood infection, a lung abscess, and even death.
Influenza is also a dangerous condition for elders. It is a viral infection that affects a person’s respiratory organs – lungs, nose, and throat. It is commonly referred to as the “flu.” Influenza is an airborne infection. Therefore, in the long-term care setting, at nursing homes and assisted living facilities, it easily spreads through coughing, sneezing, and ever mere breathing. Most of the time, people recover from influenza without complications. However, in some cases, especially for seniors whose immune systems are weakened, this infection can lead to pneumonia with potentially fatal consequences.
The Novel Coronavirus (COVID-19)
[Update as of March 2020]
The novel Coronavirus (also referred to as “COVID-19”) is a deadly virus, which started in China and, by March 11, 2020, has become a global pandemic. According to the Centers for Disease Control and Prevention (CDC), most people are able to recover from the novel coronavirus without being hospitalized. Unfortunately, CDC also warns the older people and those with chronic diseases (such as diabetes, heart disease, and lung disease) are at higher risk of suffering severe complications as a result of COVID-19. The elderly people are the most defenseless and vulnerable to this virus in terms of their risk of death. In California, elder care institutions have a history of citations due to infection control deficiencies. Therefore, in the current COVID-19 outbreak, assisted living facilities and nursing homes constitute high risk environments for the elderly.
The symptoms of the novel coronavirus include, but are not limited to, the following:
- Cough
- Fever
- Shortness of breath and difficulty breathing
- Persistent pain in the chest
- Pressure in the chest
- Confusion
- Inability to arouse
- Bluish face or lips
These symptoms require immediate medical attention.
For more information regarding the Coronavirus statistics, the discussion of California elder care institutions’ history of infection control failures, and the ways proper infection control methods can help in preventing the spread of COVID-19, read the firm’s blog article entitled “California Nursing Homes and Assisted Living Facilities are Not Prepared for the New Coronavirus Pandemic”.
Take Action! Promptly Contact a Los Angeles Nursing Home Infections Lawyer for a Free Consultation
As the Los Angeles nursing home infections lawyer, Dmitriy Cherepinskiy, and his firm, aggressively pursue justice. If you or your loved one suffered an infection at a nursing home or an assisted living facility, this firm will fight zealously to vindicate your rights. If an infection at an assisted living facility or a nursing home caused the death of a loved one, your compassionate Los Angeles assisted living infections attorney will battle tirelessly in a wrongful death case.
If you suspect elder abuse in the form of the failure to prevent or treat an infection, please call or fill out an electronic contact form today to request a free consultation. Cherepinskiy Law Firm, as the Los Angeles nursing home infections attorney, will work tirelessly to bring the wrongdoers to justice, and to obtain the maximum case value and compensation you deserve.
This firm fight for clients throughout California, including Los Angeles, Orange County, as well as Ventura, Riverside and San Bernardino Counties.
Sources
1. https://health.gov/hcq/prevent-hai.asp
2. “Infectious Diseases in the Nursing Home Setting: Challenges and Opportunities for Clinical Investigation”, Clinical Infectious Diseases (October 2010): https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3083824/
3. “Common infections in nursing homes: a review of current issues and challenges”, Aging Health (December 2011): https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3526889/
4. “Atypical Presentation of Scabies Among Nursing Home Residents”, The Journals of Gerontology: Series A, Volume 56, Issue 7 (July 2001): https://academic.oup.com/biomedgerontology/article/56/7/M424/559178/