Pressure Ulcers: Guide By – Los Angeles Nursing Home Bed Sores Lawyer
 Pressure sores are preventable. One common question people ask is: “Can you sue a nursing home for bed sores?” The answer is: if they were caused by neglect, absolutely! When bed sores develop or worsen, this is frequently a sign of elder abuse & neglect. As Los Angeles nursing home bed sores lawyer, Cherepinskiy Law Firm is an expert in this field, and his firm will zealously advocate for the rights of the pressure sore victims or their families.
Pressure sores are preventable. One common question people ask is: “Can you sue a nursing home for bed sores?” The answer is: if they were caused by neglect, absolutely! When bed sores develop or worsen, this is frequently a sign of elder abuse & neglect. As Los Angeles nursing home bed sores lawyer, Cherepinskiy Law Firm is an expert in this field, and his firm will zealously advocate for the rights of the pressure sore victims or their families.
Decubitus Ulcers and Other Terminology Applicable to Pressure Injuries
If assisted living facilities, nursing homes, and hospitals do not utilize proper preventative measures, older individuals who have cognitive impairments (e.g. dementia) and/or physical limitations (e.g. inability to reposition themselves in bed without assistance, incontinence, and poor blood circulation) are at a significant risk of developing bedsores. These pressure injuries are commonly known as “pressure sores”, “pressure ulcers”, “bedsores”, “bed sores” as well as the purely medical term “decubitus ulcers”.
What Causes Bedsores in Nursing Homes?
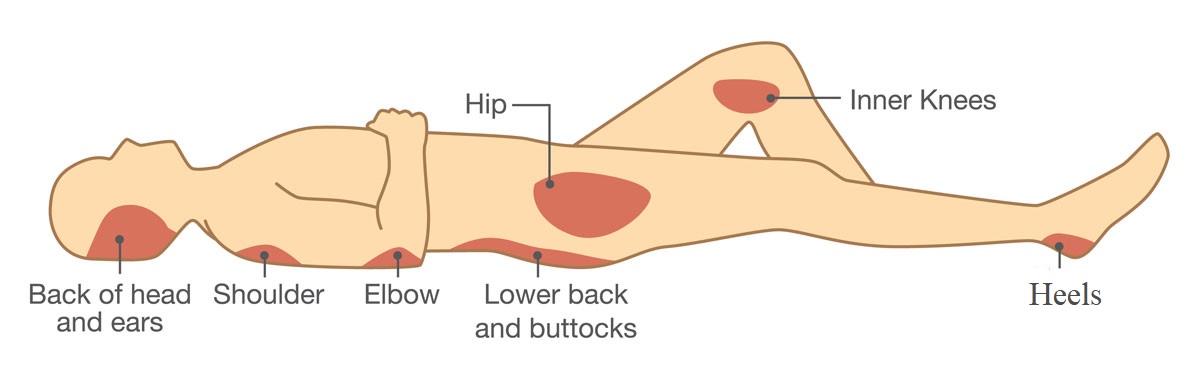
Lack of movement and pressure on the skin (typically, over a bony prominence) cause reduced blow flow which, in turn, leads to degenerating, red, and frequently painful skin areas or open ulcers – i.e. bed sores. Pressure sores can be worsened by friction, shearing (when skin and the bone underneath move in opposition directions), and exposure to feces, urine, and other irritating fluids and substances which are in contact with the person’s skin. The areas of the body that are most susceptible to bedsores are – the back side of the head, hips, sacrum (the triangular bone in the lower back located between the two pelvic hipbones), back, as well as shoulders, elbows, ankles, and hills. When evaluating cases, a Los Angeles nursing home bed sores attorney would review the pertinent medical records describing the condition of these areas during the suspected period of neglect.
Can Bed Sores Occur at Hospitals?
If one asks, “can bed sores occur at hospitals?”, the answer is – yes, unfortunately, hospitalized patients frequently develop pressure ulcers. It should not happen, but it does. In fact, pursuant to the current guidelines established by the Centers for Medicare and Medicaid Services (“CMS”), the development of a bed sore by a hospitalized patient is referred to as a “never event” – meaning that hospital patients must never develop pressure ulcers. Per these guidelines, hospitals do not receive any reimbursement from Medicare for any additional care and treatment that has to be provided to patients who develop bed sores at those hospitals.
Risk Factors for Pressure Ulcer Development
The risk of pressure ulcer development is increased for those patients who have any of these conditions:
- History of pressure ulcers: If a person had a Stage III or Stage IV pressure ulcer, and that ulcer healed, the area of the closed ulcer is predisposed to a new pressure ulcer (bed sore). Specifically, the process of decubitus ulcer closing occurs through formation of scar tissue and creation of a new epithelial surface [epithelialization]. The “new skin” that forms in the area of the healed ulcer is much more fragile than the healthy “original skin” that used to be in the affected area before the first pressure ulcer ever developed.
- Existing pressure ulcer: If a patient has a current pressure ulcer, there is a high risk that: 1) the current ulcer will get worse or 2) this patient will develop a new bed sore in another area of the body.
- Conditions affecting Mobility: Lack of mobility (immobility), and the potential for staying in the same position for a prolonged period of time – represents one of the primary risks associated with developing pressure ulcers. There are multiple conditions affecting mobility which include, but are not limited to, the following:
-
- Neurologic disorders and conditions – e.g. stroke, Parkinson’s Disease
- Spinal cord injuries (discussed below)
- Brain injuries
- Dementia
- Myocardial Infarction
- Use of Physical Restraints
- Use of Chemical Restraints
- Renal disease (chronic kidney disease) and the impaired mobility during extended periods of dialysis treatment
- Prolonged immobility in a hospital setting due to: ventilator support, lengthy surgeries and operating room (OR) stays
- Diabetes (also called “diabetes mellitus”): Diabetes impairs blood circulation (because high glucose levels damage blood vessels) and causes neuropathy (a peripheral nerve damage that manifests itself as weakness or numbness). As a result, diabetes increases a patient’s risk of developing pressure ulcers.
- Peripheral vascular disease (PVD): This disorder affects blood circulation, because it causes narrowing and blockage of veins and arteries. Due to the compromised blood flow to lower extremities, patients with peripheral vascular disease are susceptible to developing pressure ulcers involving their feet, especially the heels.
- Conditions affecting perfusion: Such conditions as heart failure, dehydration, and sepsis affect blood perfusion of various organs, including patients’ skin. As a result, those individuals who suffer from poor perfusion are at a higher risk of pressure ulcer formation.
- Spinal cord injury: Patients with spinal cord injuries typically suffer from impaired mobility and incontinence (loss of bladder and bowel control). In addition, patients with such injuries experience sensory deficits – i.e. decreased or lost sensation and inability to feel touch, cold or heat. As a result, patients with spinal cord injuries are significantly predisposed to developing pressure ulcers (bed sores).
Scales for Pressure Ulcer Risk Assessment
The assessment of pressure ulcers using standardized scales is extremely important for a variety of reasons:
- The scales are helpful in terms of generating care plans for patients, because they enable treaters to focus on those aspects that create the highest risk of developing or worsening pressure ulcers;
- This process creates a universal method of communication, which is easily understood by healthcare providers and caregivers;
- The standardized assessment scales provide a method to objectively identify and quantify the specific risks of developing pressure sores. Specifically, this assessment process allows care providers differentiate between patients who are at no risk at all, as well as those whose risk of developing a pressure ulcer is mild, moderate or high.
Some risk assessment scales have been in use for almost fifty years. In the United States, there are two commonly accepted risk assessment scales for pressure ulcers development: (1) the Braden Scale and (2) the Norton Scale. Over the years, both of these scales have been shown to be accurate, valid, and reliable.
The Braden Scale consists of six sub-scales as follows:
1. Moisture;
2. Activity;
3. Sensory Perception;
4. Nutrition;
5. Mobility; and
6. Friction and Shear.
The Friction & Shear category is scored from 1 to 3, and the rest of the categories are scored from 1 to 4. A lower score represents the highest level of impairment and the lowest level of functioning, which represents a higher risk for the development of pressure ulcers. The total scores on the Braden Scale range from 6 (as the lowest possible score) to 23 (as the highest possible score). In general, the total Braden Scale scores reflect the following risk levels:
-
- Severe risk: less than 9
- High risk: 10 to 12
- Moderate risk: 13 to 14
- Mild risk: 15 to 18
Individuals whose total score is higher than 18 are typically considered to be “not at risk” for developing pressure ulcers.
The Norton Scale consists of five sub-scales as follows:
1. Mental Condition;
2. Physical Condition;
3. Mobility;
4. Activity; and
5. Incontinence.
The sub-scales are scored from 1 (as the lowest score) to 4 (as the highest score). Similarly to the Braden Scale, based on the Norton Scale, a lower score indicates the lowest level of functioning and a higher risk in terms of developing a pressure sore. The total scores on the Norton Scale range from 5 (as the lowest possible score) to 20 (as the highest possible score). Typically, the total Norton Scale scores reflect the following risk levels:
-
- Very high risk: less than 10
- High risk: 10 to 14
- Medium risk: 14 to 18
- Low risk: more than 18
The Braden and Norton are not the only two pressure ulcer risk assessment scales. Various academic institutions and medical facilities have developed their own scales. In terms of identifying specific patients who are at risk of developing a pressure ulcer, it does not matter what specific scale is utilized – as long as a reliable risk assessment scale is used.
Bed Sore Stages
As the Los Angeles nursing home bed sore lawyer, this firm is interested in the latest developments related to the staging and treatment of pressure sores. In 2016, the National Pressure Ulcer Advisory Panel updated the definitions of pressure injuries of the skin. With respect to their stages, decubitus ulcers are divided into 4 categories (“stages”) depending on the level of skin and tissue damage:
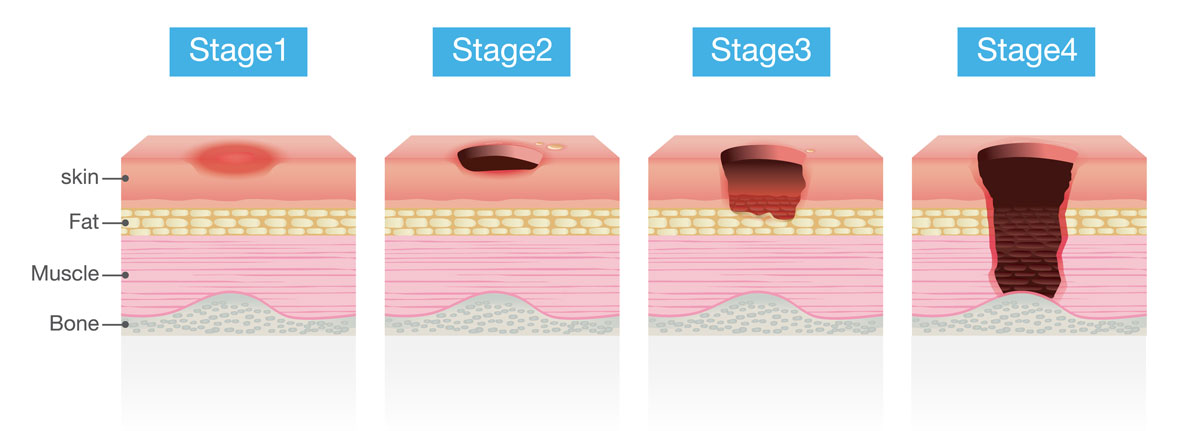
Stage 1 Bed Sore
A Stage 1 bed sore is formally defined as a non-blanchable erythema – an area of red but still intact skin, which does not lose redness when pressed. The affected area may become painful and differ in firmness or temperature when compared to adjacent tissue.
Stage 2 Bed Sore
A Stage 2 pressure ulcer involves partial-thickness skin loss with exposed dermis – i.e. the wound blisters or ruptures leading to the opening of the inner layer of the skin that contains nerve endings, blood vessels, hair follicles, and other structures. The wound frequently appears as a dry or shiny shallow sore without any visible slough (non-vital yellow skin) or eschar (dead tissue that falls off the surface of the skin).
Stage 3 Bed Sore
A Stage 3 bed sore is defined as a full-thickness skin loss — the skin is lost completely showing fat and the formation of new tissue (granulation). Sometimes, slough or eschar can be visible as well. Bones, muscles, and tendons are neither visible nor palpable.
Stage 4 Bed Sore
A Stage 4 bedsore occurs when there is a full-thickness skin and tissue loss – i.e. the ulcer becomes so deep that tendons, ligaments, muscles, or even bones become visible or palpable.
Unstageable Pressure Injury
In some cases, when the severity of the wound cannot be assessed due to the presence of slough or eschar, these ulcers are called “unstageable pressure injury”. The removal of sough and/or eschar reveals the extent of the tissue damage – typically, a Stage 3 or Stage 4 pressure ulcer.
Deep Tissue Pressure Injury (also referred to as “DTP” or “DTPI”)
This injury is defined is an area of persistent purple, deep red, or maroon discoloration of intact or non-intact skin, which does not lose redness when pressed (i.e. it is non-blanchable). A very severe injury (such as Stage 3, Stage 4, or unstageable pressure ulcer) is diagnosed when the wound is so deep that muscles, bones, tendons, ligaments, or necrotic (dead) tissue becomes visible.
Prevention of Pressure Ulcers: Explained by – Bed Sore Lawyer Los Angeles Residents Can Count On
In terms of skin care, the main goal is to prevent pressure sores because, once they develop, healing can take months or even years. In fact, if bedsores are not treated, they can become infected and lead to gangrene, sepsis, septic shock, and even death.
Elder care institutions such as nursing homes and assisted living facilities must properly and comprehensively evaluate each patient / resident’s level of mental and physical functioning, including the risk of skin breakdown, mobility, nutrition & hydration, and cognitive status. In addition to ensuring adequate staffing levels, facilities must develop appropriate and individualized Care Plans providing for timely repositioning, skin care, proper nutrition, and other measures aimed at bed sore prevention. In cases involving pressure ulcers, a Los Angeles nursing home bed sores lawyer will be looking for evidence of elder care facilities’ failures to take steps to prevent bed sores from appearing or worsening.
Repositioning
Repositioning remains the “gold standard” method of pressure ulcer prevention. Bedbound nursing home patients and assisted living residents must be repositioned from their back to the sides every 2 hours, at a minimum. Repositioning relieves pressure over those areas that are over bony prominences and are, therefore, more susceptible pressure injuries – back of the head, ears, coccyx (tailbone), buttocks, hips, shoulders, elbows, heels, inner knees, and ankles.
Typical Areas of Human Body Which Are Susceptible to Pressure Sores
Those providing care to elderly individuals (assisted living caregivers and nursing home staff) have to use appropriate techniques when turning & repositioning and avoid friction-causing methods such as dragging residents / patients along their beds. If necessary, a special draw sheet must be used for repositioning.
Those who spend most of the day in a wheelchair must be provided assistance with repositioning on an hourly basis, and they should be encouraged / assisted to shift their weight at least 3-4 times per hour. Elderly individuals who are still able to ambulate on their own must be encouraged to walk or, at least, stand as much as possible. Standing & walking keeps pressure off vulnerable areas and prevents the formation of pressure sores.
Proper Skin Care
Caregivers must provide head-to-toe skin assessments of nursing home patients and assisted living residents on a daily basis. Special attention must be paid to the most vulnerable areas – back of the head, coccyx (tailbone), hips shoulders, elbows, heels, and ankles. When washing, a soft sponge or cloth should be used. Moisturizing creams and skin protectants should be applied to the skin every day. When washing elderly people, their bodies must not be scrubbed, and talc powder and/or strong soaps must be avoided.
Nutrition and Hydration
Consumption of proper amounts of calories, protein, vitamins, and minerals is crucial for maintaining healthy skin and preventing bedsores. Drinking plenty of water every day and staying hydrated is equally important. If nursing home patients and assisted living residents have physical and/or mental impairments, they must be provided with the appropriate encouragement, guidance and, if necessary, physical assistance with meals and fluid intake in order to ensure adequate nutrition and hydration.
Pressure-Reducing Mattresses
As the Los Angeles nursing home bed sore lawyer, Cherepinskiy Law Firm cannot underemphasize the importance of prevention of bed sores through the use of pressure reducing devices. There are multiple special mattresses, which serve as “pressure-reducing” devices designed to treat or prevent bedsores (pressure ulcers). The following types of mattresses work by relieving pressure points through a redistribution of a patient’s weight:
- Non-Powered Pressure Reduction Mattress – uses various components such as foam, air, fluid, or gel to achieve friction reduction and pressure distribution. These mattresses typically feature a waterproof covering, as well as a special construction that facilitates air channeling.
- Alternating Pressure Mattress – consists of several air-fillable sections or tubes. These inflatable cells inflate and deflate in an alternating fashion. When one cell deflates, the adjacent one inflates, and the process repeats. As a result, an alternating pressure mattress prevents constant points of pressure on a patient’s body, and facilities constant “movement” of pressure from one part of the body to another.
- Low Air Loss Mattress – is a type of an air mattress. The mattress itself has thousands of very small holes. These holes are very small and they let the air out at a super slow rate. While the mattress is letting air out through the holes, an air pump provides a constant airflow into the mattress. This process essentially makes a patient “float” on top of the low air loss mattress, which reduces friction and pressure, prevents a build-up of moistures, and maintains skin temperature at normal levels.
- Alternating Pressure Mattress with Low Air Loss – this type of a mattress combines the features of both an alternating pressure mattress and a low air loss mattress.
- Lateral Rotation Mattress – utilizes a special mechanism that rotates a bed-bound patient from one side to another. It is extremely helpful in terms of preventing and treating pressure ulcers (bed sores), because it relieves and redistributes pressure, prevents excessive shear and friction, and regulates moisture and body temperature.
Pressure-Reducing Mattress Overlays
Mattress Overlays (also called “Mattress Toppers”) – represent a less expensive alternative to “full” pressure-reducing mattresses described above. These mattress overlays are placed on top of the regular mattresses. There are several types of mattress “toppers”, which are as follows:
- Air Mattress Overlays (also referred to as “air pads”) – are intended to assist those pressure sore patients who need moderate or mild pressure relief. Air mattress overlays are either permanently filled with air or kept continuously inflated with the use of an air pump. Air mattress overlays are cheaper than alternating pressure mattresses. However, they do have one key disadvantage – instead of “alternating pressure”, these overlays apply softer but constant pressure on a patient’s body.
- Alternating Pressure Overlays – are placed on top of regular mattresses and utilize the same “mechanism” as alternating pressure mattresses. Specifically, these pads contain multiple air-fillable pockets, which “take turns” inflating and deflating. Alternating pressure pads can also be equipped with a low air loss system that regulates the levels of skin temperature and moisture. Despite being less expensive than pressure-reducing mattresses, alternating pressure overlays are almost as effective in preventing or healing of pressure ulcers.
- Foam Mattress Overlays: In terms of mattress pads and covers, foam has been widely used for over sixty years. Typically, cellulose and polyurethane are used to manufacture foam mattress overlays. The most common surface shape of foam pads is called the “eggshell” or “egg crate”, due to its peak-and-valley appearance and resemblance to egg cartons you see in grocery stores. Foam overlays make the “top” of a mattress softer and provide some pressure reduction, although they are definitely not as effective in preventing or treating bed sores as air overlays and alternating pressure overlays.
- Gel Pads – are mattress overlays, which are infused with gel. In addition to reducing pressure, gel pads efficiently reduce moisture build-up between the surface of the overlay and the patient’s skin. For some patients, gel and foam overlays are used together in order to provide a more effective method of pressure relief.
- Sheepskin Pads – are another type of a mattress overlay used as a method of bed sore prevention. Due to the hollow fibers in its wool and its absorbency, sheepskin provides unparalleled level of temperature regulation and moisture control. For example, sheepskin seat covers have been used by car owners for decades. Sheepskin overlays can be more expensive than gel or foam overlays, but they can last for a long time without losing their effectiveness or shape.
Heel Pressure-Reducing Boots and Devices
Pressure-relief mattresses and mattress overlays are most effective in terms of preventing and treating pressure ulcers in such areas as the coccyx, buttocks, hips, shoulders, and the back of the head. However, the protection of heels and ankles of patients with limited mobility requires a different type of pressure-relieving device. Specifically, the following devices reduce pressure by raising the foot and keeping it suspended in air (floating) off the mattress surface:
- Heel sleeves;
- Heel pillows;
- Heel suspension positioners, boots and protectors. For example, one such commonly used device is a Prevalon Heel Protector, which is typically referred to as the “Prevalon Boot”. Its bottom has a special cushion that allows the patient’s heel to be suspended over the surface of a mattress or a mattress overlay.
Other Bed Sore Prevention Methods
The following clothes increase the risk of developing pressure sores and must be avoided: clothes that are very tight and/or clothes with buttons, zippers, and thick seams which can press on the skin. In addition, clothes should not wrinkle or bunch up in the areas that are susceptible to pressure injuries – e.g. coccyx (tailbone), hips shoulders, elbows, heels, and ankles.
After urination or a bowel movement, the area must be cleaned and dried very well. Excessive moisture in the genital and pelvic area can quickly lead to the formation of a pressure sore. Bedridden patients must never be allowed to lay for hours in their urine and feces which, unfortunately, does happen in some extreme cases of nursing home neglect involving incontinent patients.
As discussed above, foam mattresses or those filled with gel / air help in preventing bed sores, as well as a soft cushion or foam placed between parts of the body that press against each other or the bed. When a patient is lying on a side, a pillow or a soft cushion helps with pressure reduction if placed between ankles and knees. If a resident is bedridden, when lying on his / her back, soft pillow or a foam cushion should be placed under the following areas: coccyx (tailbone), shoulders, elbows, and heels or calves. Bed sheets have to be smooth and dry (without wrinkles).
Any sharp or hard objects, such as pencils, pens, coins, must be removed from the patient’s bed. Finally, the head of the bed should not be elevated higher than a 30-degree angle for the following reason: if the head of the bed is raised higher than 30 degrees, it causes people to slide down which, in turn, causes shearing and increases the risk of skin breakdown.
Overall, it is very important for a legal professional to know the medicine related to the prevention, assessment, and treatment of bedsores. When seeking justice, always look for a bed sore lawyer Los Angeles residents trust as a knowledgeable specialist.
Appropriate Staffing Levels Help with Pressure Ulcer Prevention
A nursing home – acquired bed sore can quickly lead to catastrophic consequences. Preventing bed sores in nursing homes must be administrators’ first priority. When a nursing home generates an adequate care plan, but it is understaffed – i.e. it simply does not have sufficient staff members to reposition patients, assist with nutrition & hydration, and provide other pressure ulcer preventative measures – the care plan becomes meaningless. The methods for pressure ulcer prevention must be used in conjunction with appropriate numbers of qualified staff members.
Treatment of Pressure Sores: Overview by – Los Angeles Nursing Home Bed Sore Lawyer
Treating pressure ulcers is very difficult, and it requires a multi-modality approach. Less severe (lower stage) bedsores may heal within several weeks with appropriate treatment. However, very significant (high stage) open ulcers may take months or even years to heal, may require a surgery and, in some tragic cases, may never heal leading to a fatal outcome.
Several treatments are commonly utilized to promote the healing of pressure ulcers. An overview of these bed sore treatments, as provided by the Los Angeles nursing home bed sores lawyer at Cherepinskiy Law Firm, is as follows:
Pressure Reduction
Pressure relief and reduction is the simplest method of pressure ulcer control. The pressure is removed from the sore by repositioning / moving a resident. Another pressure relief method involves the use of pillows, cushions, or foam pads to support and prop up the affected parts of the patient’s body.
Wound Cleaning and Dressing
Pressure ulcers must be clean and dry to promote healing. Relatively minor sores may be cleaned with water and the gentle application of mild (not strong) soap. Open pressure ulcers must be washed with a solution of saline every single time the wound dressing is changed. Timely changed and carefully applied wound dressings serve to speed up the healing process and protect wounds from infections. Therefore, dressing changes play an important role in the treatment of pressure sores. In analyzing a potential case, a Los Angeles bed sore attorney would review the medical records to see what type of dressing was used for a particular patient. The specific types of wound dressings are described below.
Types of Dressings for Treatment of Pressure Ulcers
Various dressings used to treat pressure ulcers include, but are not limited to, the following (in alphabetical order):
- Absorbent Compress dressings: These dressings are designed for the treatment of wounds, which produce a significant amount of exudate (a fluid that is produced during the process of wound healing). Absorbent dressings consist of multiple layers of absorptive material such as cotton, rayon, or cellulose. One of the layers is a “non-adherent” layer, which means it does not “stick” to the wound and promotes faster healing. These dressings are highly effective, because they protect pressure ulcers from external environment and bacteria, stay dray for long periods of time, and do not need to be frequently changed.
- Alginate dressings also have significant absorbent characteristics. The active component in this type of dressing is calcium sodium alginate or calcium alginate (a biodegradable substance manufactured from seaweed). When an alginate dressing is applied to a pressure ulcer, it creates a gel substance that forms a moist protective cover over the wound and promotes faster healing.
- Antimicrobial dressings consist of a dressing or gauze with low-adherent properties, which is saturated with an antimicrobial ointment.
- Capillary Action dressings are used to treat wounds (including pressure ulcers), which generate heavy exudate. These dressings are made using hydrophobic fibers (e.g. acrylic, polyester, and modacrylic), as well as outside layers with low-adherence properties. Capillary action dressings remove wound exudate and, at the same time, maintain sufficient moisture for enhanced wound healing.
- Transparent Film dressings are made with polymer membranes, which are adherent (i.e. have an adhesive) on one side. These dressings specific permeability characteristics (i.e. allowing to be passed through and penetrated). Specifically, firm dressings are not permeable to water, liquids, and bacteria and, at the same time, they are permeable to oxygen and moisture vapor. The transparent nature of these dressings allows pressure ulcers to be visualized. These dressings are primarily used for partial-thickness pressure ulcers that produce insignificant or no exudate.
- Foam dressings are made of polymer foam (typically, polyurethane) with cells designed to hold fluids. In order to allow for easy and non-traumatic removal, the wound-contacting surface of foam dressings is non-adherent. These dressings are intended to be used for pressure ulcers involving full-thickness and partial-thickness wounds.
- Honey‐Impregnated dressings are made with medical grade honey (e.g. Manuka honey or active Leptospermum). Due to the anti‐inflammatory and antimicrobial characteristics of medical grade honey, these dressings can be utilized to promote healing of acute wounds as well as chronic wounds (such as pressure ulcers).
- Hydrocolloid dressings are made with gel-forming chemical components such as gelatin or pectin. These dressings are designed to be used for uninfected wounds, including pressure ulcers. Hydrocolloid dressings don’t require frequent changes, have a waterproof backing, and form an insulating and most environment that aids in wound healing.
- Hydrogels are made out of approximately 90% water contained in a gel base, and the remaining approximately 10% is plant-based starch polymer. The primary function of hydrogels is to keep a pressure ulcer moist, thereby protecting the wound from an infection and promoting the healing process. Besides their “treatment” function, hydrogels also provide pain relief. Although hydrogels are an ointment, they are considered to be a “dressing” and are made in the following forms:
-
- amorphous hydrogel – an ointment in the form of a pure gel;
- hydrogel sheet dressing – a gel, which is made in combination with a specific type of thin fiber mesh; and
- impregnated hydrogel dressings – special gauzes, sponges (made without weaving), strips as well as ropes that are saturated with hydrogel.
- Iodine‐Impregnated dressings are dressings, which are saturated with Povidone Iodine that gets released into the wound. Iodine has very strong antimicrobial properties, and it is very effective in neutralizing bacteria and fungi. Iodine has been used in wound care for over 150 years.
- Low‐Adherence dressings are typically pads (made out of cotton), which are placed on a wound. The pads can be either medicated or non-medicated. The medicated dressings are saturated with an ointment or a medication. Examples of non-medicated dressings are:
-
- Saline gauze dressing
- Paraffin gauze dressing
- Odor Absorbent dressings contain a layer of activated charcoal, which absorbs toxins and bacteria, and neutralizes odors from pressure ulcers and other wounds affected by infections, fungi, and necrosis. In addition, odor absorbent dressings use cyclodextrin that works by absorbing odor-generating molecules.
- Protease‐Modulating Matrix dressings (also called “PMM dressings”) is intended to remove protease (an enzyme that breaks down peptides and proteins) from wound fluids. Medical scientists indicate that in some cases, slow wound healing can be due to high levels of protease. By removing protease from the wound, PMM dressings promote faster wound healing.
- Silver‐Impregnated dressings are utilized in the treatment of infected wounds, including pressure ulcers. Silver has antimicrobial characteristics, and it is effective in reducing and controlling the spread of bacteria.
- Soft Polymer dressings are made with a soft polymer (typically, silicone polymer) that has non-adherent or low-adherent properties. Soft polymer dressings offer moderate absorbency and can be used for wounds producing moderate or heavy exudate.
Types of Topical Agents for Pressure Ulcers – Creams and Ointments
Wound ointments and creams, which are also referred to as “topical agents”, are either 1) placed directly on a pressure ulcer and covered with gauze or dressing or 2) impregnated into dressings and placed on wounds. The following are the most common types of creams and ointments utilized in the treatment of decubitus ulcers (pressure sores):
- Amorphous Hydrogel ointment (discussed above)
- Cadexomer Iodine gel is made with a specific starch polymer that contains iodine. When this gel is applied to a pressure ulcer wound, it kills bacteria, absorbs would fluids and exudate, and removes would debris and slough.
- Collagenase ointment is a sterile debriding ointment, which is “enzymatic” in nature. Collagen represents three quarters of the weight of skin tissue. Collagenase helps the wound-healing process by digesting collagen in necrotic tissue and promoting granulation and epithelization of pressure ulcers.
- Phenytoin ointments are utilized to treat pressure ulcers (bed sores). As an oral medication, phenytoin is most commonly administered to assist with controlling epileptic seizures. However, in its “topical” form (as a lotion or a cream), this medication is believed by some researchers to have the potential to stimulate wound healing.
- Silver Sulfadiazine cream is referred to as a “sulfa antibiotic”. As a topical medication, silver sulfadiazine is applied to wounds, including pressure sores, to treat and prevent wound infections. If wound bacteria are allowed to spread, it can affect adjacent skin areas and may even enter the blood stream causing a life-threatening sepsis. Silver sulfadiazine stops bacterial growth and reduces the risk of spreading bacteria.
Pressure Ulcer Debridement (Debridement of Dead Tissue)
Dead or infected tissue prevents wound healing. Accordingly, necrotic (dead) tissue must be removed through the process of wound debridement. The founder of this firm, Dmitriy Cherepinskiy, as the Los Angeles nursing home bed sore attorney, understands the importance of wound debridement as one of the most effective methods of pressure ulcer treatment. As a method of pressure sore treatment, wound debridement is the process of removing devitalized, necrotic, or infected tissue from a pressure ulcer until surrounding healthy and normal tissue becomes exposed. This process promotes wound healing. Clinical research shows that debrided pressure ulcers have a significantly higher rate of healing than non-debrided wounds. Therefore, debridement is a very important aspect of pressure ulcer care. There are multiple different types of pressure ulcer debridement, which are as follows:
Sharp Debridement: Surgical Debridement and Conservative Sharp Wound Debridement
Both (1) surgical debridement and (2) conservative sharp wound debridement represent a procedure, which is performed with sterile surgical instruments: forceps, scalpel, scissors, curette, or rongeur. The procedure involves a sequential physical removal of devitalized tissue [i.e. necrotic or avascular tissue], which serves to promote healing of the affected wound such as a pressure sore.
-
- Surgical debridement is an aggressive and complex surgical procedure that has to be performed in specialized surgical setting with an operating room (OR) such as a hospital, a surgical center, or a wound care clinic.
-
- Conservative sharp wound debridement (CSWD) is a relatively simpler procedure that can be safely performed not only in a specialized surgical setting, but also at the bedside in a long-term care facility or even at home.
In deciding whether a patient needs to undergo a surgical debridement or a conservative sharp wound debridement, wound care specialists assess such factors as the severity of a pressure ulcer and the amount of devitalized or necrotic tissue that needs to be removed.
Mechanical Debridement
Mechanical debridement is performed with the use of a mechanical and abrasive force. This type of wound debridement removes devitalized and necrotic tissue, but it can also remove and damage viable and healthy tissue. This procedure is typically painful. The most common types of mechanical debridement are as follows:
-
- Wet-to-Dry Dressing involves application of a sterile piece of gauze saturated with normal saline to the exposed wound bed. When the gauze appears to be dry, a wound care specialist forcibly peels the gauze off the wound. The devitalized or necrotic tissue “sticks” to the gauze during the drying process and, as a result, it gets removed along with the gauze. This approach is painful, and it carries the risk of damaging healthy tissue.
-
- Whirlpool Therapy (also known as “Hydrotherapy”) is another type of mechanical wound debridement. It is utilized to perform debridement of pressure ulcers and other wounds that are infected or involve significant eschar and necrotic tissue. This method of debridement carries serious risks such as (1) tissue damage due to significant turbine forces and (2) bacterial cross-contamination – i.e. transferring of bacteria from the infected wound to healthy areas of the body.
-
- Pulsed Lavage (also referred to as “Pulsatile Jet Lavage” and “Irrigation”) is a kind of mechanical debridement, which utilizes a pulsed and pressurized solution. This process irrigates the wound and removes necrotic and devitalized tissue. During the procedure, the irrigation solution is suctioned along with the detached necrotic tissue. One of the advantages of the pulsed lavage debridement (compared to other types of mechanical debridement) is that it removes devitalized tissue and promotes tissue granulation without damaging normal and healthy tissue.
Enzymatic Debridement (Chemical Debridement)
During an enzymatic debridement procedure, a topical agent is applied to a pressure ulcer or another wound. This topical agent starts a chemical process that uses enzymes to liquefy and dissolve necrotic tissue. Enzymatic debridement is not as painful as other types of mechanical debridement, and it can be performed on a daily basis. This method of wound debridement does not require the specialized setting of a wound care clinic, and it is frequently utilized in the nursing home setting.
Autolytic Debridement
Autolytic debridement involves removal of devitalized and necrotic wound tissue through a natural process occurring in a moist environment. Specifically, in a moist environment under a wound dressing, the body’s enzymes contained within wound fluids work by disrupting proteins that bind necrotic tissue to the body. As a result, enzymes liquefy necrotic tissue. The frequency of dressing changes is important. This method is a conservative type of wound debridement, and it is typically reserved for those patients who are not candidates for more aggressive types of debridement (e.g. surgical debridement).
Autolytic debridement is the slowest type of debridement, because it takes several days for necrotic and devitalized tissue to soften up and separate. Nevertheless, it is effective and it does have several advantages over other types of wound debridement: it is comfortable and not painful, and it does not damage healthy tissue. Due to these characteristics, autolytic debridement is also routinely used in the setting of long-term care (e.g. skilled nursing facilities).
Biological Debridement
Biological debridement involves application of maggots to necrotic wounds. Maggots utilized in wound care do not carry any bacteria, because they are grown in a sterile environment. These maggots are the larvae of Lucilia Sericata (the green bottle fly). They secrete a specific digestive enzyme, which breaks down the necrotic and devitalized wound tissue. In the natural setting, the larvae of the green bottle fly feed on decaying organic tissue (e.g. dead animals). When applied to a wound bed and covered with a dressing, sterile maggots essentially “eat” necrotic tissue and bacteria.
Incontinence Control
Genital and pelvic area moisture prevents the healing of pressure ulcers, and in fact, makes the patients’ condition worse. Therefore, incontinence must be controlled as much as possible.
Antibiotics and Antibacterial Medications
If pressure ulcers do now show signs of healing within two weeks or appropriate wound care (timely wound cleaning and dressing), antibacterial medications may be prescribed to promote healing. If pressure sores become infected, then antibiotics must be administered either as oral medications or in the form of antibiotic creams and ointments.
Vacuum-Assisted Therapy
Negative pressure wound therapy (which also referred to as the “vacuum-assisted therapy” or “wound VAC” procedure) can be a very effective treatment technique for bed ulcers. Due to its simplicity and effectiveness, this modality has seen increased use and popularity during the recent years. A piece of foam is inserted into the pressure ulcer, a perforated drain is placed on top, and the entire area is firmly covered. Then, the open end of the drain tube is connected to a vacuum-creating device, and fluid is drawn from the sore into a special reservoir. The removal of fluid reduces colonization of bacteria and the risk of infections, thereby facilitating wound healing and significantly improving healing time.
Surgery
Unfortunately, some bed sores become so critical and severe that a surgery becomes inevitable. A surgical procedure called “flap reconstruction” involves taking a muscle, skin, or tissue from a healthy area of a patient’s body and grafting / placing it over the pressure ulcer. The goal of surgical intervention is to reduce the risk of further infection and other complications by cleaning and covering the wound.
Take Action! Promptly Contact a Los Angeles Nursing Home Bed Sores Attorney for a Free Consultation
Pressure ulcers are preventable wounds. Therefore, if a nursing home patient or an assisted living resident develops a pressure sore or it gets worse (i.e. deteriorates to a higher stage), it is frequently the sign of nursing home neglect or assisted living neglect. Untreated bed sores can become infected and lead to gangrene, sepsis, septic shock, and even wrongful death. When it comes to nursing homes, understaffing is typically one of the main reasons patients are neglected to the point when they develop bed sores. If a resident of an assisted living facility develops a pressure ulcer, usually, this means that the facility accepted or retained a resident who needed a higher level of care than this assisted living facility was licensed and able to provide.
If you suspect or believe that you or your loved one’s pressure ulcer(s) was /were caused or aggravated by the negligent or reckless misconduct on the part of a nursing home or an assisted living facility, it is crucial to immediately consult with a Los Angeles nursing home bed sores attorney. Please call or fill out an electronic contact form today to request a free consultation. Cherepinskiy Law Firm will work tirelessly to make sure the wrongdoers are brought to justice, and to obtain the maximum compensation through a resolution or a trial.
This firm provides legal services for the pressure sore victims and their families throughout California, including Los Angeles and Orange Counties, as well as Riverside, San Bernardino, and Ventura Counties.
Sources
1. https://medlineplus.gov/pressuresores.html
2. https://medlineplus.gov/ency/patientinstructions/000147.htm
3. https://www.cdc.gov/nchs/products/databriefs/db14.htm
4. https://www.cms.gov/newsroom/press-releases/bed-sores-can-be-stopped-proper-care-nursing-homes-medicare-project-shows